Is Your Canker Sore a Sign You Have Coronavirus?

In the early months of the COVID-19 pandemic, we fussed over every cough and sniffle. Since then, we’ve gone through several variants of the virus, each presenting a unique set of symptoms.
As we continue to ride the rollercoaster that is COVID-19, new fears and anxieties are sure to crop up, especially related to unexpected health issues
Before COVID-19 emerged, you may not have given your canker sores a second thought other than, “Ugh, this again?” But now, it’s easy to worry that issues like mouth sores are related to COVID-19.
So, are canker sores a sign of COVID? Let’s explore the potential connection between the two.
About COVID-19
It’s important to have accurate information about COVID-19 that’s backed by scientists and health professionals. Only then can we answer the question, are canker sores a sign of COVID?
There are many different types of viruses you can be exposed to on any given day. Some of these viruses lead to disease, and some don’t. Coronaviruses are a family of viruses that lead to disease, usually of the respiratory variety. You may remember hearing news of the panic over the SARS coronavirus, or SARS-CoV, that ensued in the early 2000s.
In 2019, a new coronavirus was discovered: SARS-CoV-2. The term COVID-19 refers to the disease a person gets after contracting the virus SARS-CoV-2.
COVID-19 is an infectious disease that spreads from person to person through tiny particles that carry the virus. These particles float into the air when an infected person breathes or talks, and more are released if the person laughs, coughs, or sneezes.
The smaller the particles, the longer they linger in the air, and the more people they can affect. If an indoor space has poor ventilation, these particles remain in the space, and they can pile up and stick to surfaces for longer periods of time.
For the virus to travel from person to person, the expelled particles from one person enter the body of another person through the air they breathe. The virus can also enter the body via contact with a contaminated surface. You might touch the surface and then touch your mouth, nose, or eyes, where the virus can enter your body.
Once inside your body, the viral infection hijacks healthy cells, usually starting with your throat and the inside of your nose, causing cold- and flu-like symptoms.
In some cases, the virus continues to spread to your lungs, hijacking and killing more healthy cells. The resulting symptoms resemble those of pneumonia. As it becomes more difficult to breathe, your lungs may lose function, and you may need to be put on a ventilator to assist with breathing while your lungs heal.
The trouble with mechanical ventilation is the accompanying risk of bacterial infection. At this critical stage, if you contract a bacterial infection, you could suffer from organ failure and eventually death.
Even a mild or symptom-free case of COVID-19 could result in long COVID or long-term damage, including blood clots and other issues with blood vessels.
Common COVID-19 Symptoms
COVID-19 particularly affects the upper respiratory tract, including the sinuses, nose, and throat, as well as the lungs and windpipe. Most people who contract COVID-19 have mild symptoms, but others become severely ill.
The most common COVID-19 symptoms appear 2–14 days after exposure to the virus. These include:
- Fever or chills
- Fatigue
- Cough
- Shortness of breath
- Muscle and body aches
- Loss of taste or smell
- Congestion
Other more intense symptoms indicate the need for immediate emergency medical care, including:
- Trouble breathing
- Pressure in the chest
- Confusion
- Difficulty staying awake
- Pale, gray, or blue skin and lips
- Low blood oxygen
Remember, with each new variant, different symptoms have been reported, so it’s important to stay educated on the latest information. But are canker sores a sign of COVID, as well? Let’s take a quick look at canker sores and how they form.

About Canker Sores
Canker sores, also known as aphthous ulcers, are lesions that form inside your mouth. They only form on soft tissues, including the insides of your cheeks or lips, the roof of your mouth, along the gumline, and under your tongue.
Several activities might damage the inside of your mouth and lead to a canker sore. These include:
- Biting your cheek
- Brushing too hard
- Getting hit in the face
- Sustaining an injury from dental work
Certain foods can also trigger canker sores, even if you’re not allergic to them. Acidic foods and spicy foods can distress the soft tissue in your mouth, leading to an ulcer. And if you already have a canker sore, it’s important to avoid acidic and spicy foods to let it heal — and to spare yourself unnecessary pain.
Other causes of canker sores include a weakened immune system, hormonal fluctuation, vitamin deficiency, genetics, and stress. No matter the cause, canker sores are not contagious and usually heal on their own within a week or two.
Canker Sore Symptoms
Fortunately, canker sore symptoms are relatively easy to identify. Canker sores remain inside the mouth (unlike cold sores) and don’t typically cause other side effects.
Minor canker sores, which account for about 80% of canker sore cases, are small, pale, and oval-shaped with a red or pink border.
Major canker sores are larger and deeper, with irregular edges. These sores can last over two weeks and grow to over one centimeter in diameter. Adults usually experience extreme pain and difficulty eating and drinking during major canker sore outbreaks.
Herpetiform canker sores are tiny but occur in large clusters that may combine into one large ulcer. They can develop in many places in the mouth, including on the inside of the lips, on the roof of the mouth, inside the cheeks, under the tongue, and at the base of the gums. These usually heal in one to two weeks.
Occasionally, canker sores can even develop on the tonsils or in the back of the throat. These mouth sores display distinct red edges and a yellow, gray, or white center. The pain caused by a canker sore in the throat is often so severe that it’s mistaken for strep throat or tonsillitis, though it isn’t dangerous.

Are Canker Sores a Sign of COVID?
Now that you know more about COVID-19 and canker sores, we can really explore their connection. Are canker sores a sign of COVID?
While the two health problems don’t sound related, canker sores could indicate an underlying coronavirus infection — just not for the reason you’d expect.
There’s no evidence that COVID-19 directly triggers canker sore ulcers, but the stress and trauma of a coronavirus infection could manifest itself in a way that triggers canker sores. Anecdotal evidence and clinical research suggest a high correlation between canker sores and stress, anxiety, and depression.
The pandemic has challenged our mental health. During this time, you may have mourned the loss of a loved one, dealt with isolation, worried for your safety or the safety of others, experienced financial hardship, or grieved the loss of your pre-pandemic routine. These significant and difficult changes can undoubtedly lead to stress, anger, fear, and depression.
As a result, you may have had trouble sleeping, struggled to control existing health problems, or turned to unhealthy habits to cope. These are common reactions to stress and trauma, but they can weaken your immune system. Without a strong immune system, your body struggles to properly fight antigens and invaders. This is why you always seem to become more susceptible to illnesses when you’re under intense stress.
With its unpleasant symptoms and its disruptions to our lives, it’s no wonder COVID-19 can make people more vulnerable to canker sore outbreaks.
Other Mouth Ulcers May Be COVID-19 Symptoms
So, are canker sores a sign of COVID? They can be — and so can other ulcers.
Canker sores are just one type of ulcer that can develop inside your mouth. And while cankers aren’t identified as a common or direct symptom of COVID-19, some other mouth ulcers are.
Before the pandemic, oral ulcers were mainly associated with trauma to the mouth or an underlying condition. Now, they’ve been linked to COVID-19 through a phenomenon called COVID tongue.
Oral symptoms associated with COVID-19 include a persistent, white film on the tongue, a furry tongue, geographic tongue, and painful lesions or rashes on the tongue or inside the mouth. Patients may experience only one of these symptoms or several at once.
Many COVID patients have reported having COVID tongue, especially those who develop a severe infection. In a small study, researchers found that up to 11% of COVID patients at a hospital in Madrid experienced COVID tongue.
Research published by the British Journal of Dermatology also demonstrates this trend. More than 300 of the 666 patients studied presented signs of COVID tongue, which included burning sensations, ulcers, painful red and white bumps, and swelling.
Because of its less obvious nature compared to more serious symptoms, COVID tongue was not initially identified as a symptom of COVID-19. However, it’s now well known as a consistent COVID side effect.
If you’re experiencing unfamiliar discomfort in your mouth or if you’ve noticed the appearance of your tongue changing, take a COVID test and talk to your doctor or dentist right away.
Is It Time to See a Doctor?
Now that we’ve answered the primary question (are canker sores a sign of COVID?), you may be wondering whether you need to see a doctor.
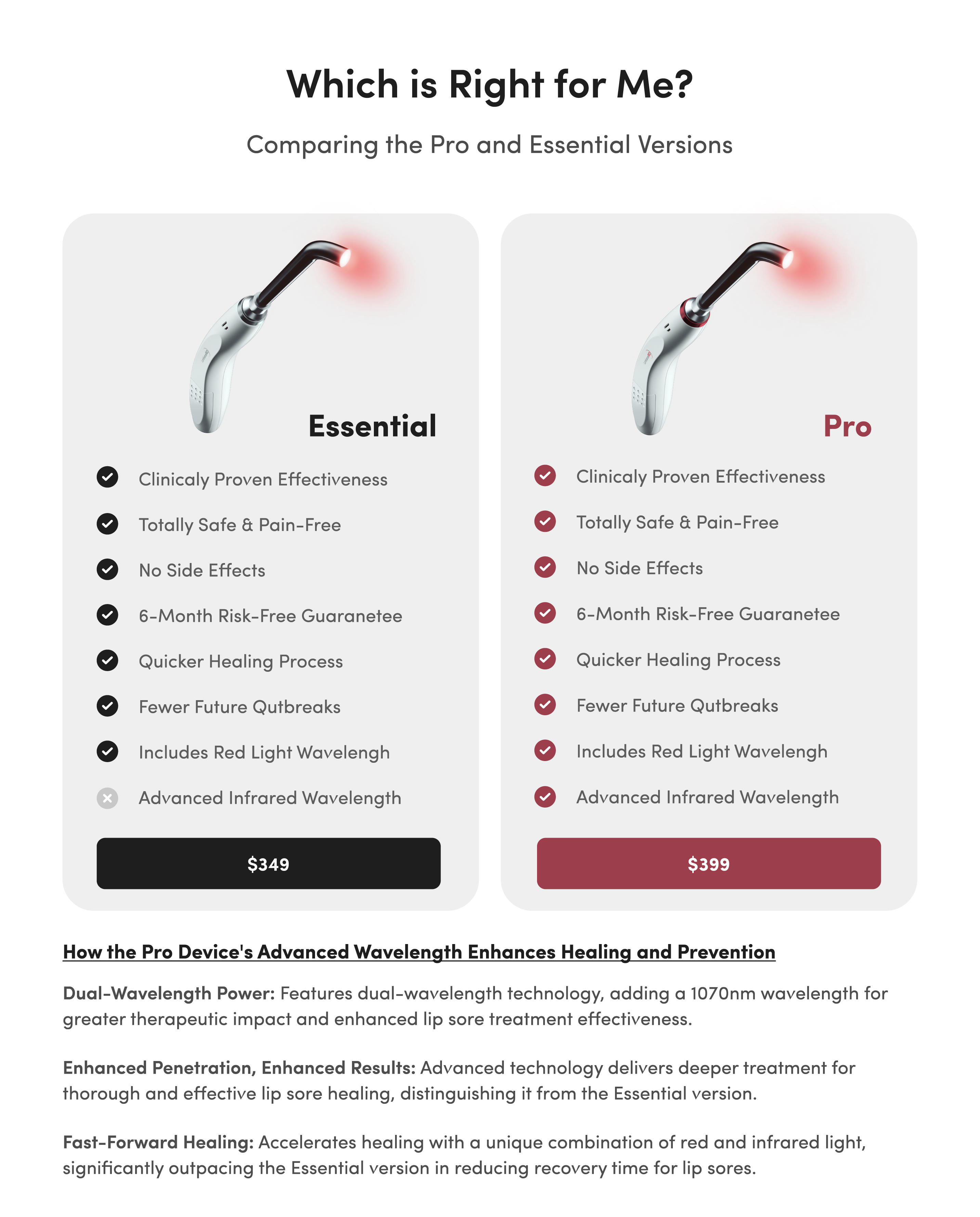
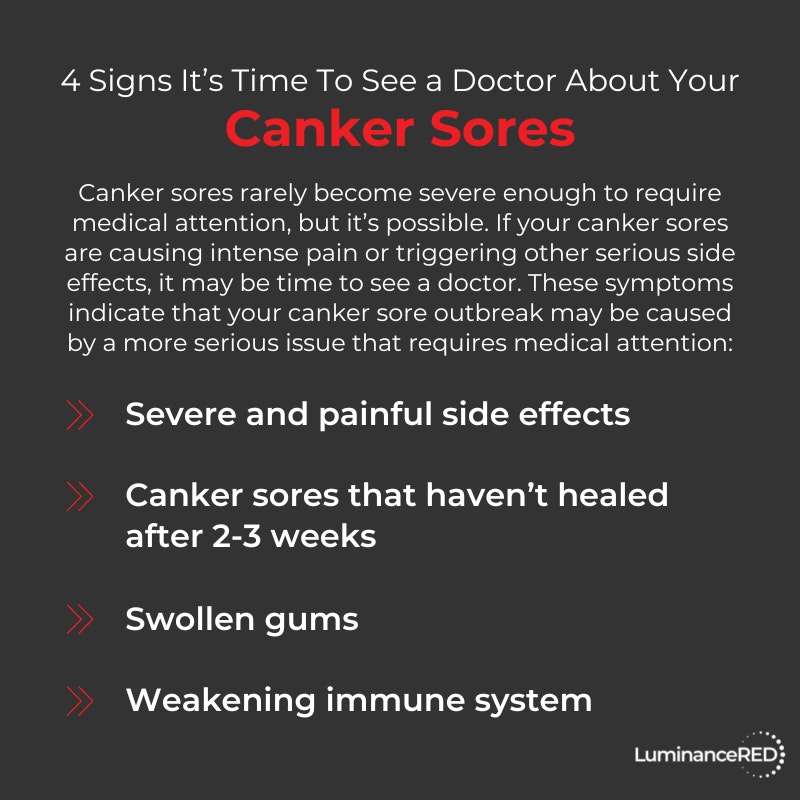
Canker sores rarely become severe enough to require medical attention, but it’s possible. If your canker sores are causing intense pain or triggering other serious side effects, it’s best to see a medical professional.
The symptoms below indicate that your canker sore outbreak may be caused by a more serious issue that requires medical attention:
- Severe and painful side effects
- Canker sores that haven’t healed after two to three weeks
- Swollen gums
- Weakening immune system
Also see a doctor if you’re experiencing other COVID-19 symptoms in addition to a canker sore. Trouble breathing, persistent pressure in the chest, confusion, and bluish lips are four COVID-19 symptoms that require immediate medical attention.
Once you’ve been assessed, a doctor will determine whether you should be treated in the hospital or sent home to quarantine.
Finally, if you haven’t already, talk with your physician about receiving a COVID vaccine or the next available booster shot.