The Ultimate Genital Herpes FAQ

So, you were recently diagnosed with genital herpes. Or, you started dating someone with herpes, and you’re worried about contracting it. Or, you’ve been exposed, but you don’t yet know whether you’re infected.
Regardless of your specific situation, you’re likely overwhelmed with questions you’ve never had to ask before: What exactly is herpes? Is there a cure? Where do genital herpes appear? What can be mistaken for genital herpes? How often do genital herpes outbreaks occur?
The more you know about genital herpes, the better you’ll feel — and we have all the answers you need right here.
What Is Herpes?
The herpes simplex virus (HSV) is a common virus that causes cold sores and genital herpes.
Cold sores are usually caused by the herpes simplex virus type 1 (HSV-1), while genital herpes is more often caused by the herpes simplex virus type 2 (HSV-2). HSV-1 and HSV-2 are both members of the Herpesviridae family of DNA viruses, so they share many characteristics and symptoms, including recurring outbreaks of painful sores.
It was once believed that only HSV-2 caused genital herpes via sexual transmission, but researchers now estimate that half of genital herpes cases in females are actually caused by HSV-1, not HSV-2.
Different Types of Herpes
Oral herpes and genital herpes are the two most common and well-known types of herpes infection.
Oral Herpes
Oral herpes spreads through direct contact with skin and mucous membranes, typically causing cold sores to develop on the face around the lips or mouth. A cold sore is highly contagious, especially when oozing blisters are present, and may be spread by kissing, touching faces, or sharing a drink, among other means of transmission.
After the initial outbreak, HSV-1 remains dormant in your nerve cells until a trigger reactivates it. The virus may lie inactive for weeks, months, or even years, though there is no cure. It’s hard to predict exactly when and how a person’s next oral herpes outbreak will occur.
Genital Herpes
Genital herpes is a sexually transmitted infection without a known cure. The most common sign of genital herpes is the development of blisters around the genital area, such as the groin, rectum, or upper thighs. Herpes blisters are often itchy and can be painful.
Genital herpes is highly contagious, especially during an active outbreak. However, you can spread the herpes virus to others even when you have no symptoms at all due to asymptomatic shedding.
What Does Herpes Look Like?
Cold sores emerge around the lips or mouth and pass through five distinct phases: tingling, blistering, weeping, crusting, and healing.
Genital herpes, on the other hand, produces small red bumps and white blisters grouped closely together on, around, or inside the genital region. These blisters may appear days or weeks after your first exposure to the virus and may last two to six weeks.
You may notice tingling, itching, or burning as genital herpes blisters develop. These sores become very painful, fill with fluid, then burst, dry out, and scab over. Though it may take a few weeks, most genital herpes scabs heal without any scarring.
How Far Away Is a Cure for Herpes?
Unlike bacterial infections, which can be quickly cleared with antibiotics, a viral condition like genital herpes has no available cure.
Our best hope for a genital herpes cure may come not from a shot, but from genome editing using something called CRISPR technology.
In December 2019, scientists at Harvard Medical School successfully disrupted the herpes simplex virus for the first time and identified weak spots where the virus may be susceptible to gene editing. Early indications suggest there’s hope, but a viable cure is likely years or even decades away.
How Many People Have Herpes?
The percentage of people with herpes varies based on location, age, and demographic, but overall, herpes is a widespread and common disease. Oral herpes is more prevalent than genital herpes.
Worldwide, the percentage of people with one or both viruses is estimated to exceed 90%.
How Many People Have Oral Herpes?
According to the World Health Organization (WHO), an estimated two-thirds of people under the age of 50 are infected with HSV-1. That’s more than 3.7 billion people, or 67% of the world’s population. HSV-1 also impacts nearly 50% of all American men and women aged 14–49.
How Many People Have Genital Herpes?
According to the WHO, 417 million people worldwide aged 15–49 are infected with HSV-2.
It is believed that about 140 million people worldwide are infected with genital HSV-1, especially in the Americas, Europe, and the Western Pacific.
Altogether, more than half a billion people worldwide have a genital herpes infection. In the United States alone, one out of every six people aged 14–49 has genital herpes.
How Does Genital Herpes Spread?
Genital herpes mainly spreads through sexual contact. The risk of spreading genital herpes depends on a number of factors, some of which are within your control:
- Length of time you have been infected with the herpes virus
- Whether your partner is a man or woman
- How frequently you use condoms during sex
- Whether you take antiviral medication
In a recent study of couples in which only one partner had genital herpes and condoms were used only during outbreaks, up to 10% of uninfected partners became infected within one year.
The risk drops significantly with additional precautions, such as consistent condom use and antiviral medication. One large study reported that only 1.9% of susceptible partners became infected with clinically symptomatic HSV-2 when their infected partner took an antiviral drug as a precautionary treatment.
Women who acquire herpes during pregnancy or experience reactivation of the virus during pregnancy also have the potential to transmit herpes to their baby. Fortunately, in utero transmission is relatively rare, and only about one in 3,200 births result in HSV transmission to the baby. However, accidental transmission can occur afterward as well.
How to Get Rid of Genital Herpes
If you’ve recently experienced your first outbreak, you’re probably eager to learn how to get rid of genital herpes.
First, talk with your doctor about antiviral drug options that reduce healing time for existing herpes sores and prolong the period between outbreaks. We’ll cover antiviral medications more thoroughly below.
In the meantime, plenty of items in your home may provide relief and eliminate the symptoms of an active genital herpes outbreak. For example, coconut oil is anti-inflammatory, meaning it can reduce swelling, and an analgesic, which means it soothes pain. It’s also antiviral and antimicrobial, a great combination for fighting an outbreak.
Apple cider vinegar is another ingredient you probably have on hand. Like coconut oil, it’s antimicrobial and anti-inflammatory. Apply a mixture of one part apple cider vinegar and three parts water to genital sores (never apply undiluted vinegar to your body). Be sure to avoid contaminating the bottle.
Recent research has also backed light therapy, also called photobiomodulation, as a way to heal genital herpes sores faster and increase time between outbreaks. We’ll discuss more about how to get rid of genital herpes using light therapy at the end of the article.
Where Does Genital Herpes Appear?
Genital herpes sores may appear anywhere on your genitals. They can also appear on your groin, pubic area, upper thighs, and near, on, or just inside your anus.
During some outbreaks, you may have just a few sores around one of these areas, but a severe outbreak could cause sores in multiple areas. Herpes outbreaks tend to become less severe over time, so if you’re dealing with a bad infection, remain calm. Speak with your doctor, know that things will likely get better, and try some of the therapies mentioned here in the meantime.

How Long Does It Take for Herpes to Show Up After Exposure?
Your first herpes outbreak, known as the initial or primary infection, is usually the most severe. Some lucky people remain asymptomatic for a long period of time or forever, but it’s common to experience intense flu-like symptoms within seven to 14 days of infection.
In addition to genital sores, symptoms of an initial outbreak often include:
- Fever and chills
- Bodily aches and pains
- Headache
- Fatigue
- Swollen glands
- Difficult or painful urination
- A tingling sensation in the affected area
Expect your initial herpes outbreak to last two to four weeks. Future outbreaks are usually shorter and less painful.
How Do You Test for Herpes?
The herpes virus doesn’t always trigger outbreaks and symptoms, so testing is an important way to monitor your health. The Centers for Disease Control and Prevention (CDC) recommends testing if you are experiencing symptoms that could be related to herpes or if you recently had sex with a new partner who has genital herpes.
There are a few different ways to test for and diagnose herpes:
- Testing a tissue sample or herpes sore sample
- Conducting a polymerase chain reaction (PCR) test to look for the presence of herpes DNA
- Detecting the presence of HSV antibodies through a blood test
What Can Be Mistaken for Genital Herpes?
If you have a sore in the genital area, is it definitely herpes? What can be mistaken for genital herpes?
If you notice lesions or sores around your general area, try not to panic. It’s good to exercise caution, but get a proper diagnosis from a qualified health professional before you assume you have genital herpes.
Here are a few health conditions that can mimic the symptoms of genital herpes:
- Contact dermatitis is an itchy, irritated rash that can occur anywhere on the skin, including around your genitals. It’s an inflammatory response to direct contact with an irritating or allergy-inducing substance.
- A yeast infection can be mistaken for genital herpes because it causes itching and pain in the genital area.
- Genital warts are another common sexually transmitted disease caused by a virus, but in this case, the culprit is the human papillomavirus, or HPV. Genital warts have a different appearance than herpes sores and rarely break open or ooze.
- Syphilis causes ulcers in the genital area that can look and feel like genital herpes. Unlike herpes, syphilis comes with other symptoms, including a rash, fever, and headache. Simple testing can determine the difference, and syphilis can be cured with antibiotics.
- Molluscum contagiosum also causes lesions, but they can form on any part of the body. These distinctive-looking lesions usually heal on their own.
If you have any sort of sore, lesion, or ulcer on your body you can’t explain, consult your doctor to get a proper diagnosis.
How Often Do Genital Herpes Outbreaks Occur?
If you’ve experienced an initial herpes outbreak, your next question might be, “How often do genital herpes outbreaks occur?”
The answer is completely dependent upon the individual. Some people contract the virus and even spread it to others without even having an outbreak themselves. Others go weeks, months, or years between outbreaks. And some experience outbreaks in quick succession.
Genital herpes outbreaks can be triggered by the following:
- Sexual activity
- Menstruation
- Hormonal fluctuations
- Direct sunlight
- The common cold
- A weakened immune system
- Irritation or injury to the skin
- Fatigue
- Stress
If you think stress might be a factor in the frequency of your genital herpes outbreaks, prioritize self-care whenever possible. Practice deep breathing, meditation, or yoga. Work on your sleep routine, treat your body kindly, and make time to socialize with friends and loved ones.
How Contagious Is Herpes?
We’ve established herpes viruses are contagious, but just how contagious is herpes?
The herpes virus is always contagious, even when no symptoms exist. However, the risk of transmission increases when blisters or oozing open sores are present in the midst of an outbreak.
From the time you begin to feel the itching or burning sensation of a developing outbreak until the time your sores completely heal, consider the virus highly contagious. A sore is not considered fully healed until the scab falls off and the skin underneath returns to normal.
If you’re the susceptible partner in your relationship and don’t want to contract herpes, abstain from intimate contact until each outbreak has cleared, always use a condom during sex, and discuss antiviral therapies with your partner.
How Long Does a Herpes Outbreak Last?
Most people experience their first outbreak of genital sores about two to 12 days after initial exposure to the virus. After the blisters break, it may take up to four weeks for herpes ulcers to heal.
Subsequent outbreaks tend to be less intense and don’t usually last as long. Sores tend to heal within three to seven days during recurring outbreaks, and the number of outbreaks typically decreases over time.
How Long Does Herpes Live on Objects?
We know herpes can spread from person to person, but how long does herpes live on objects?
According to the book “Managing Herpes,” published by the American Social Health Association, herpes transmission via objects is possible, but not likely. The life of the virus on an inanimate object is estimated to be just a few hours. After that, the virus weakens and loses its ability to invade new cells.
Transmission is most likely if your genital region touches a surface — such as a towel or your fingers — that then immediately comes into contact with someone else. However, with appropriate prevention and care, this is easily avoided.
How Can You Speed Up the Healing of a Herpes Outbreak?
Antiviral medications are a key method for controlling and minimizing herpes outbreaks. There are several FDA-approved antiviral drugs available that are specifically designed to treat infections caused by the herpes simplex virus.
One such medication is particularly effective when started at the first sign of an outbreak. It works by inhibiting the replication and spread of the herpes virus during an outbreak, though it does not completely eliminate the virus from the body. Many individuals find they experience symptom relief within a few days of starting treatment.
Another antiviral option affects the virus's DNA replication over a longer period, allowing for less frequent dosing while still maintaining effective control over the outbreak.
In addition to pharmaceutical options, light therapy presents a non-drug alternative for managing genital herpes, which will be explored further below.

What Is the Science Behind Red Light Therapy for Treating Genital Herpes?
Now that you have the answers to some of the most common questions about genital herpes (Where do genital herpes appear? What can be mistaken for genital herpes? How often do genital herpes outbreaks occur?), let’s explore light therapy and its role in treating this disease.
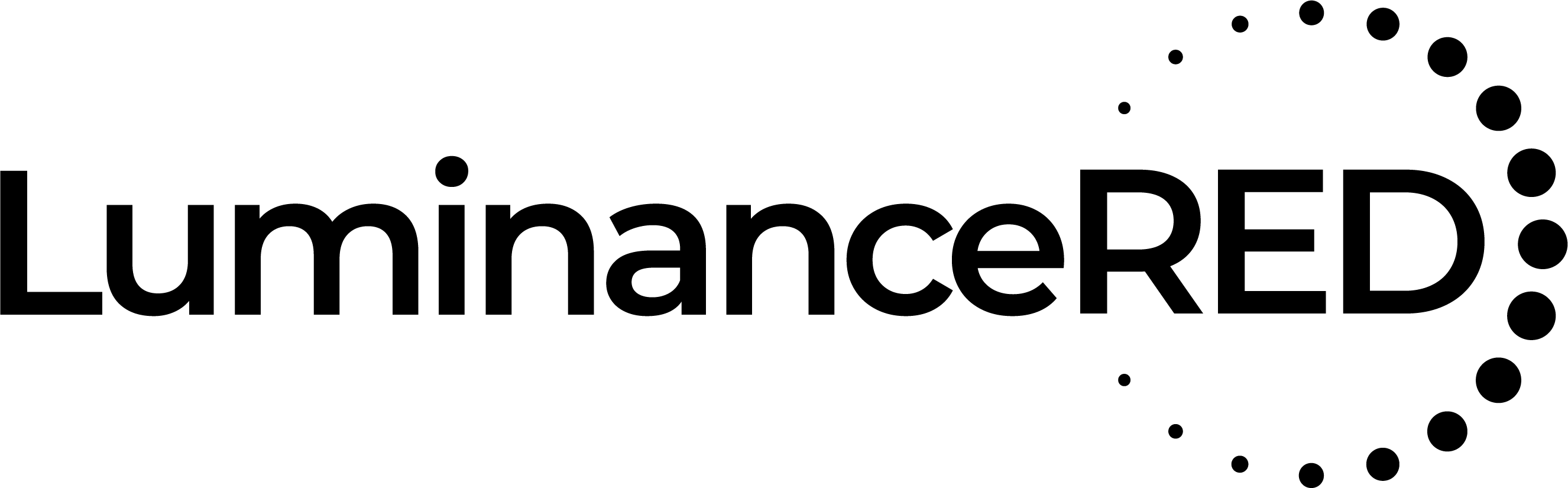
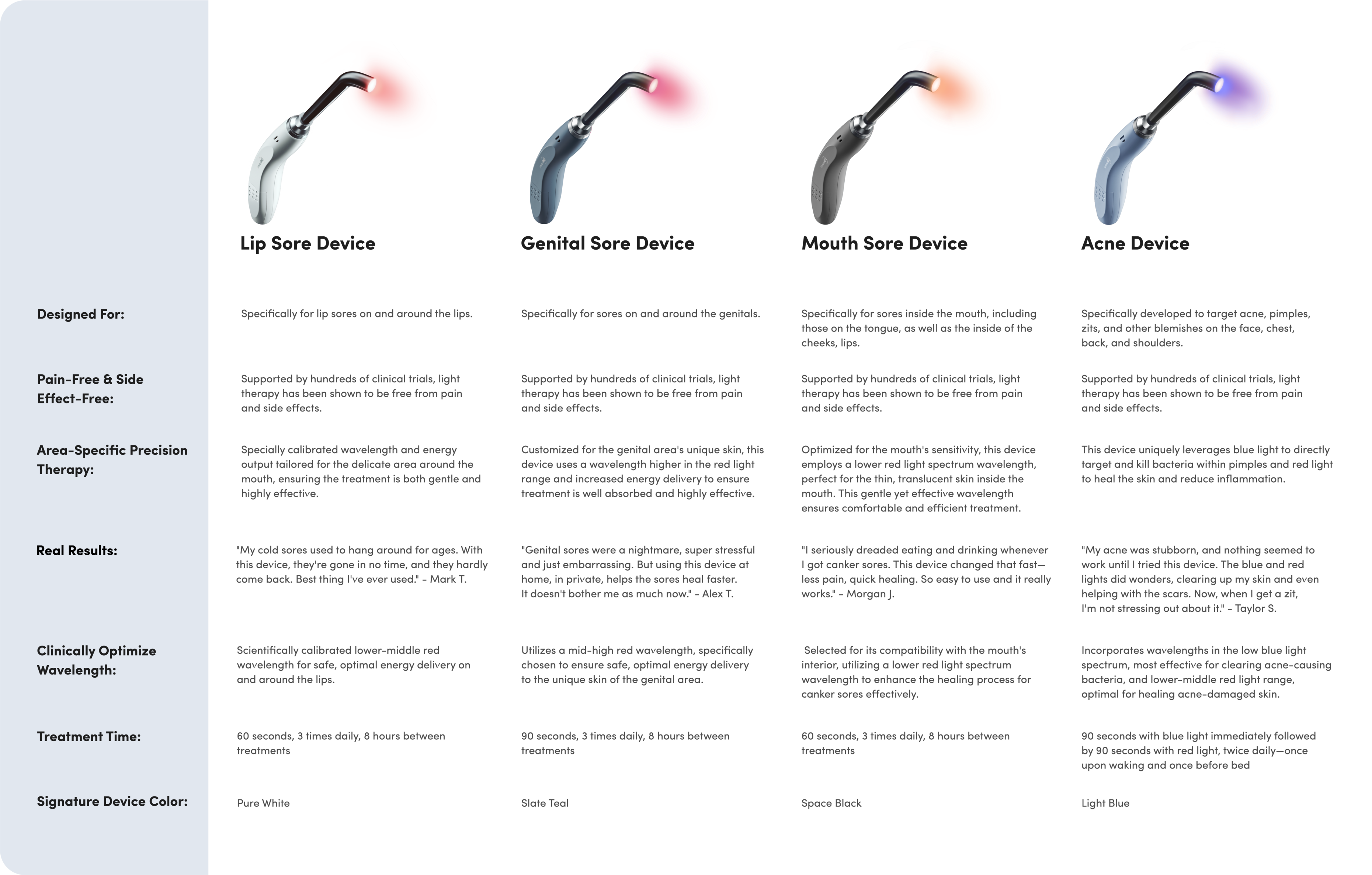
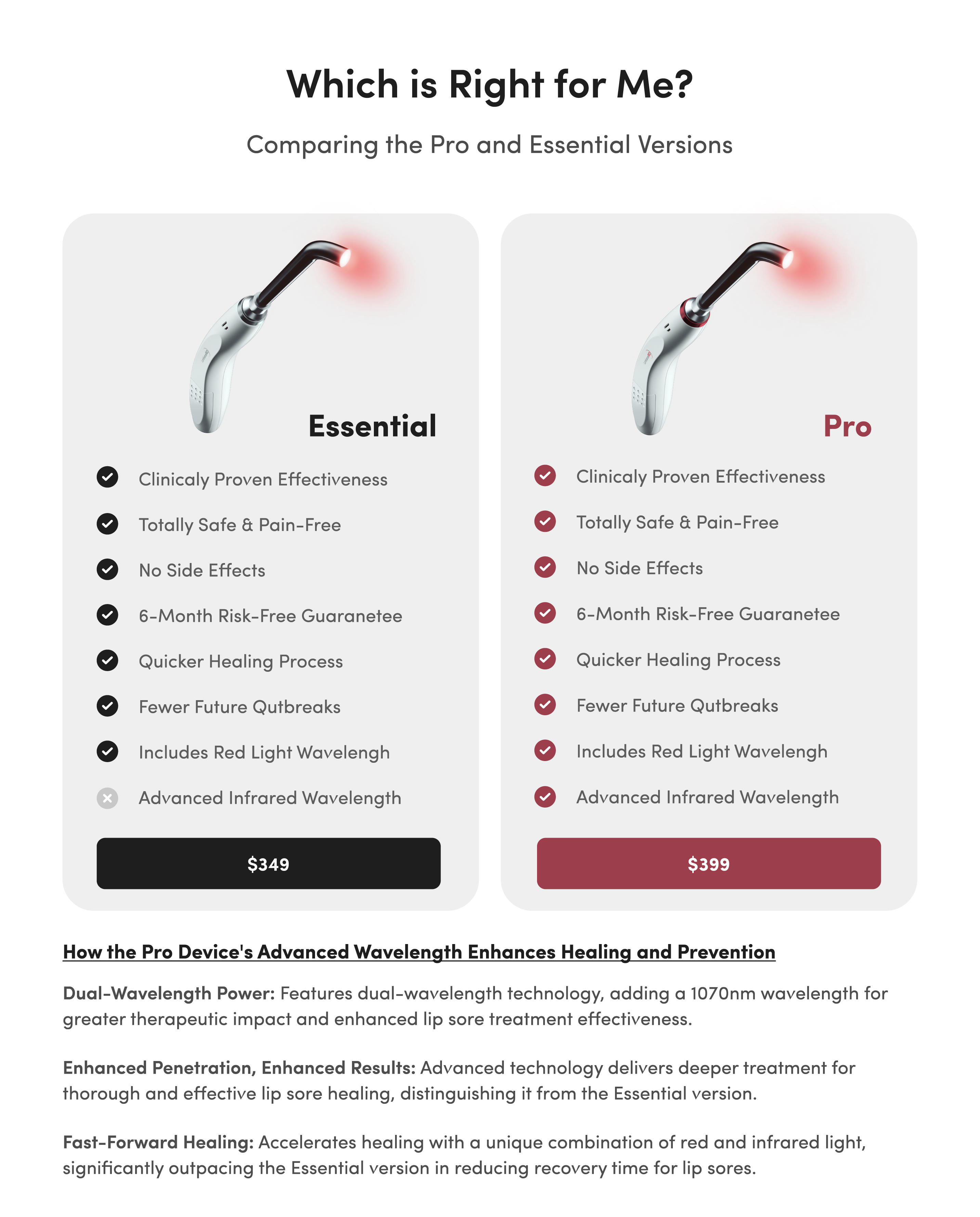
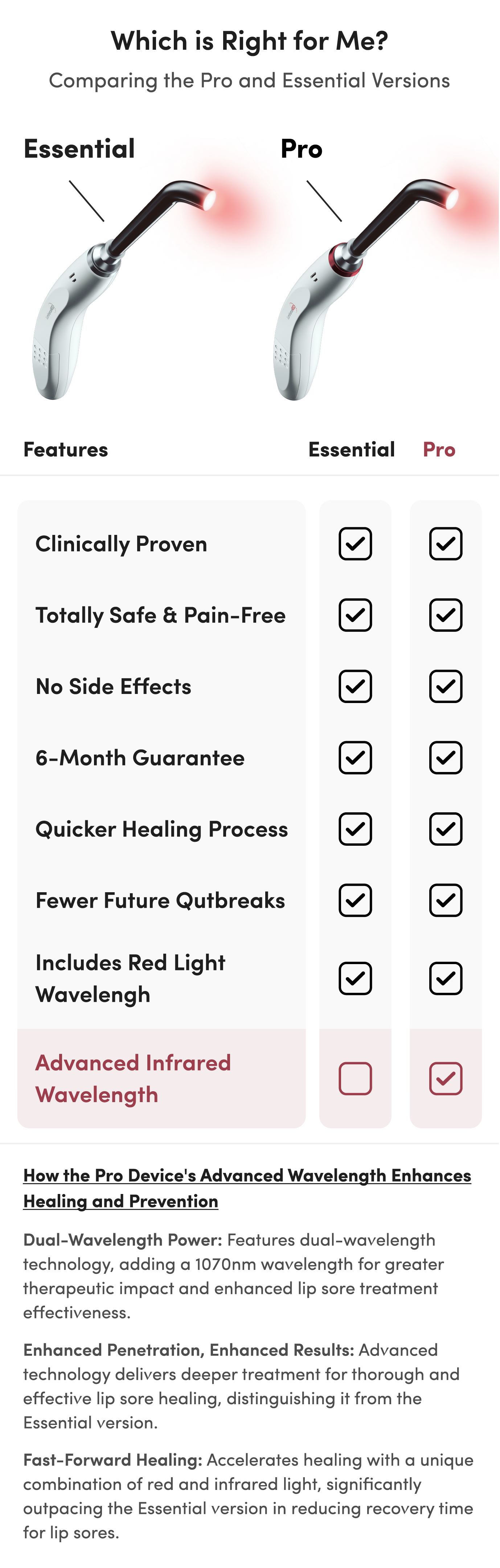
High-powered red light therapy, an emerging treatment option for genital herpes, has been clinically shown to effectively manage genital herpes outbreaks. Administered through a handheld device, such as the Luminance RED Genital Sore Treatment Device, red light penetrates skin cells to accelerate the healing process and strengthen defenses against future attacks.
Clinical data shows that regular use of red light therapy can reduce herpes-related pain, shorten the healing time of active outbreaks, and lengthen the time between future outbreaks.
With just a few 90-second treatments per day, you can discreetly take control of genital herpes from the comfort of your own home — and that’s good news for everyone.