Is There a Connection Between Coronavirus and Cold Sores?

It’s hard to remember life before COVID-19. Since March of 2020, even a simple sneeze or sniffle can cause us to worry we’ve caught the coronavirus. And people with new or worsening conditions also wonder whether their symptoms are related to the coronavirus.
If you’re prone to cold sores, you may be wondering about a potential coronavirus-cold sore relationship. Here’s what you need to know about the connection between the coronavirus and cold sores.
What Are Cold Sores?
The herpes simplex virus type 1 (HSV-1) is one of more than 100 known herpes viruses. It most commonly causes cold sore outbreaks around the lips and mouth.
The HSV-1 virus spreads during close contact with infected skin or saliva. It can enter the body through any break in the skin, even a small cut. Once inside your body, herpes lies dormant and inactive in nerve cells until activated by a trigger such as fatigue, stress, injury or hormonal changes.
Some people with HSV-1 remain asymptomatic most of their life and rarely experience outbreaks. Others experience an intense initial outbreak followed by regular monthly or yearly outbreaks for many years.
When you experience a cold sore outbreak, your sores progress through five distinct phases. These unique phases make it easy to differentiate cold sores from other conditions:
- Itching and burning develops under the skin.
- Fluid-filled blisters develop on or around the mouth.
- Blisters burst or “weep” and release their fluids.
- Cold sores dry into yellow and brown crusts.
- Scabs fall off to reveal healthy skin.
What Is Coronavirus?
Before 2020, only medical professionals knew the term coronavirus. Today it’s the most commonly used word in the English language.
Coronaviruses are actually a family of viruses that can infect people and animals. They normally cause mild to moderate upper respiratory illnesses like the common cold. Some recent coronaviruses, though, have caused more severe illnesses like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). These are dangerous, but not as widespread as the coronavirus we all know today, which causes COVID-19.
COVID-19 is an infectious disease caused by a coronavirus known as SARS-CoV-2. It affects the upper respiratory tract, including the sinuses, nose and throat, as well as the lungs and windpipe. COVID-19 spreads from person to person through droplets of saliva or discharge from the nose when an infected person sneezes or coughs. Most people who contract COVID-19 have mild symptoms that resolve on their own, but others can become severely ill.
The most common COVID-19 symptoms appear 2-14 days after exposure to the virus, including:
- Fever or chills
- Fatigue
- Muscle and body aches
- Cough
- Shortness of breath
- Loss of taste or smell
- Congestion

Can You Get a Coronavirus Cold Sore?
COVID-19 is caused by a relatively new strain of the coronavirus, so experts are still learning more about its signs and symptoms. However, cold sores are not known to be correlated with today’s coronavirus and are not reported as a likely symptom of COVID-19.
Coronavirus would not directly cause cold sores to develop around your mouth. It’s possible, though, that a coronavirus infection could weaken your immune system and trigger the herpes virus already in your body to cause a cold sore.
A weak or compromised immune system is one of the leading triggers for cold sores. When your body’s defenses come down, it’s much easier for viruses like HSV-1 to take control and cause unwanted symptoms. COVID-19 and herpes both heavily impact people with compromised immune systems.
Do You Have a Compromised Immune System?
If you are immunocompromised, meaning you have a weak or compromised immune system, you are at a higher risk of illness and infection. You may be immunocompromised if you have any of these risk factors:
- Chronic diseases like lupus, rheumatoid arthritis or type 1 diabetes
- Medical treatments that weaken the immune system, such as chemotherapy
- Regular tobacco use
- Obesity
- Old age
The effects of a compromised immune system can be significant. According to recent data, 71% of all COVID-19 patients needing hospitalization had at least one underlying health issue.
Other Common Cold Sore Triggers
While a compromised immune system could be to blame for your cold sores, other triggers play a role in cold sore outbreaks as well.
Sunlight
Sunlight is a well-established trigger for cold sores. Unprotected exposure to even relatively small levels of UV radiation can stimulate herpes virus activity. When this happens, the virus moves from its dormant resting place in the nerve ganglia and travels into cells around the lips and mouth.
Stress
Persistent mental stress and fatigue can trigger viral activity just like sunlight. This type of psychological strain actually interrupts the regulation of cellular immunity, which increases the likelihood of herpes virus reactivation.
For example, if the summer season causes significant stress in your personal life or workplace, you may see the side effects of that stress in the form of a cold sore outbreak.
Acidic Diet
The wrong eating habits also increase your risk of a long-lasting herpes outbreak. Acidic foods are some of the worst culprits because they aggravate the virus and make existing cold sores worse. If you’re prone to cold sore outbreaks, try to avoid wine, soda, tomatoes and citrus fruits at your next backyard barbeque.
Possible Connection Between the COVID-19 Vaccine and Herpes Zoster
A small new study found that the COVID-19 vaccine may trigger herpes zoster, or shingles, in some immunocompromised people. Herpes zoster isn’t “the” herpes infection you’re thinking of. It’s actually brought on by the same herpes virus that causes chickenpox: the varicella-zoster virus.
If you’ve ever had chickenpox, you might think the virus went away after you recovered from the illness. But, much like other herpes viruses, varicella-zoster doesn’t leave your body. Instead, it goes dormant inside your nerve cells. If your immune system becomes compromised, the virus can reemerge to cause shingles, which involves a very painful rash with blisters, usually on the trunk of the body.
The study analyzed side effect data from 491 people with autoimmune inflammatory rheumatic diseases after they received the Pfizer-BioNTech vaccine. A total of six patients developed mild singles within a few days of receiving the vaccine.
This sounds alarming, but according to experts, you shouldn’t panic. This doesn’t prove that the COVID-19 vaccine causes shingles. Instead, it highlights a potential link between the vaccine and shingles for certain people and underscores the need for more research.
The varicella-zoster virus is distinctly different from the herpes viruses that cause genital herpes and cold sores. It isn’t contagious when no symptoms are present, and it isn’t a sexually transmitted infection like the herpes simplex virus type 2. Herpes zoster can only develop in adults who’ve had chickenpox in the past.
When Is It Time To See a Doctor?
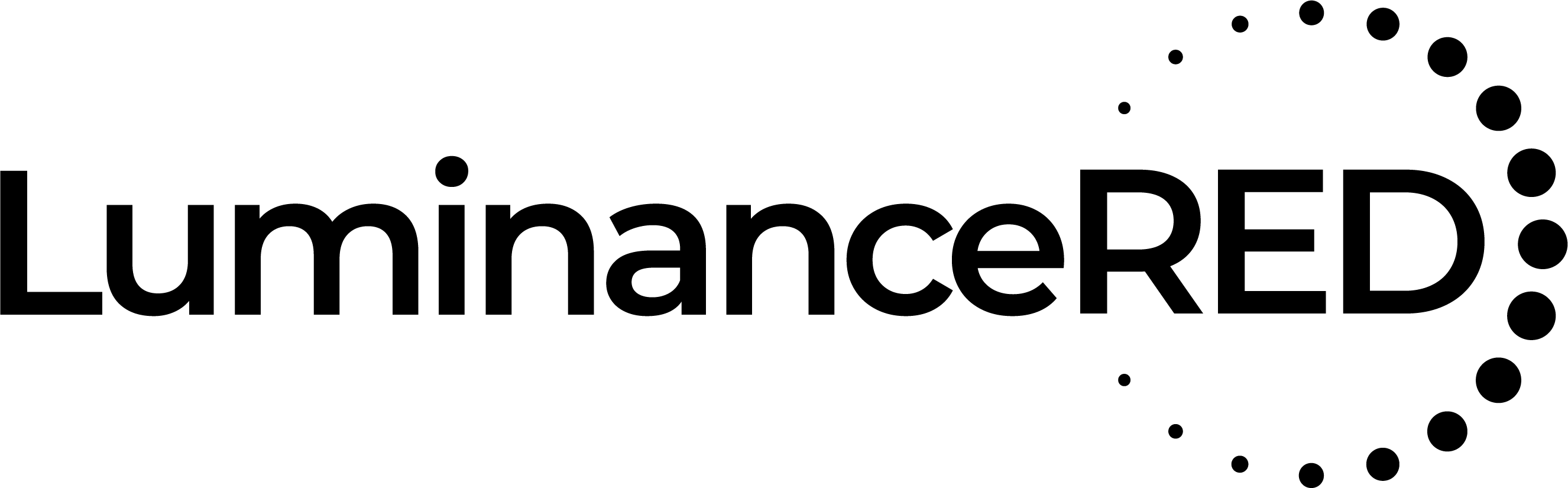
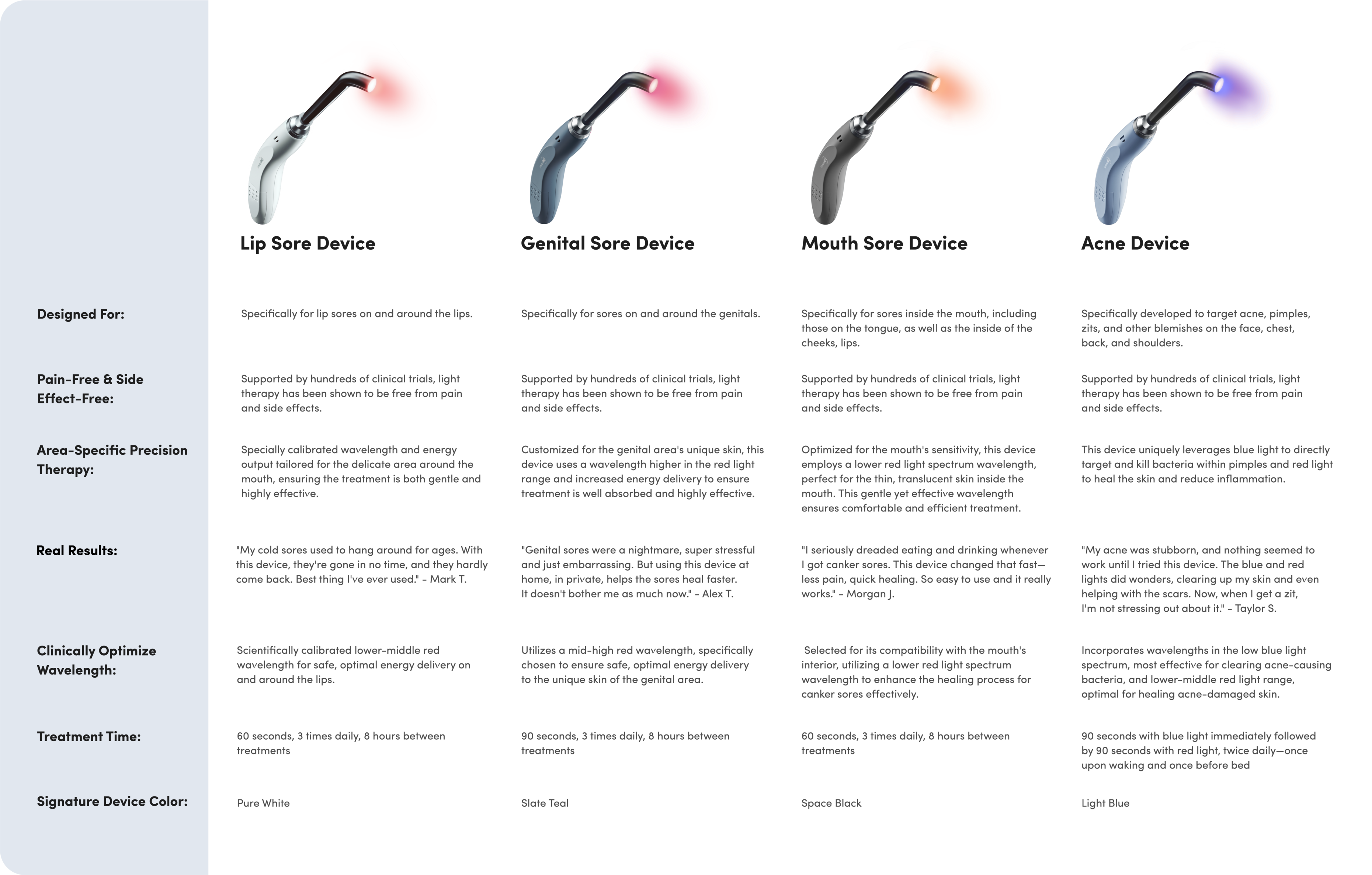
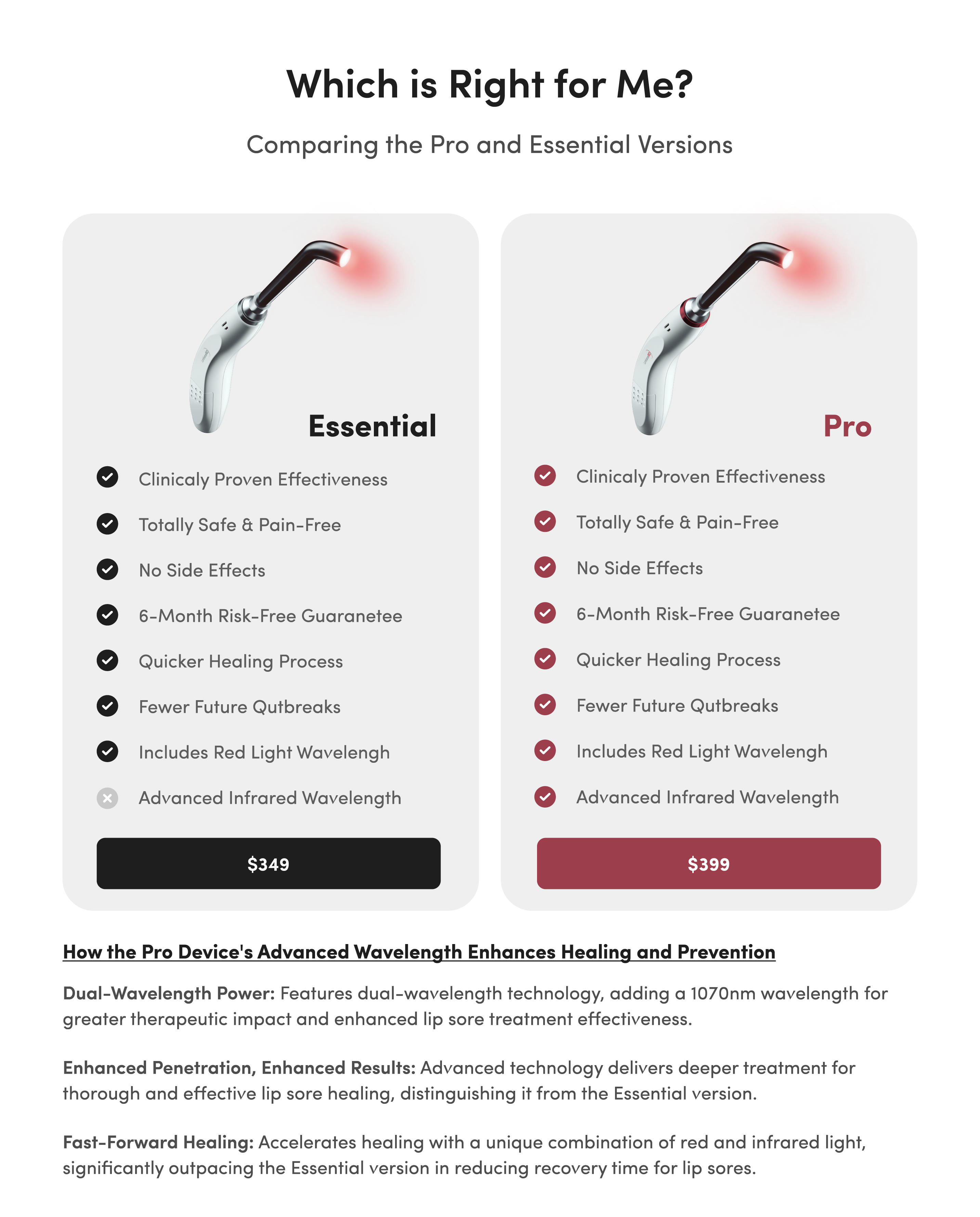
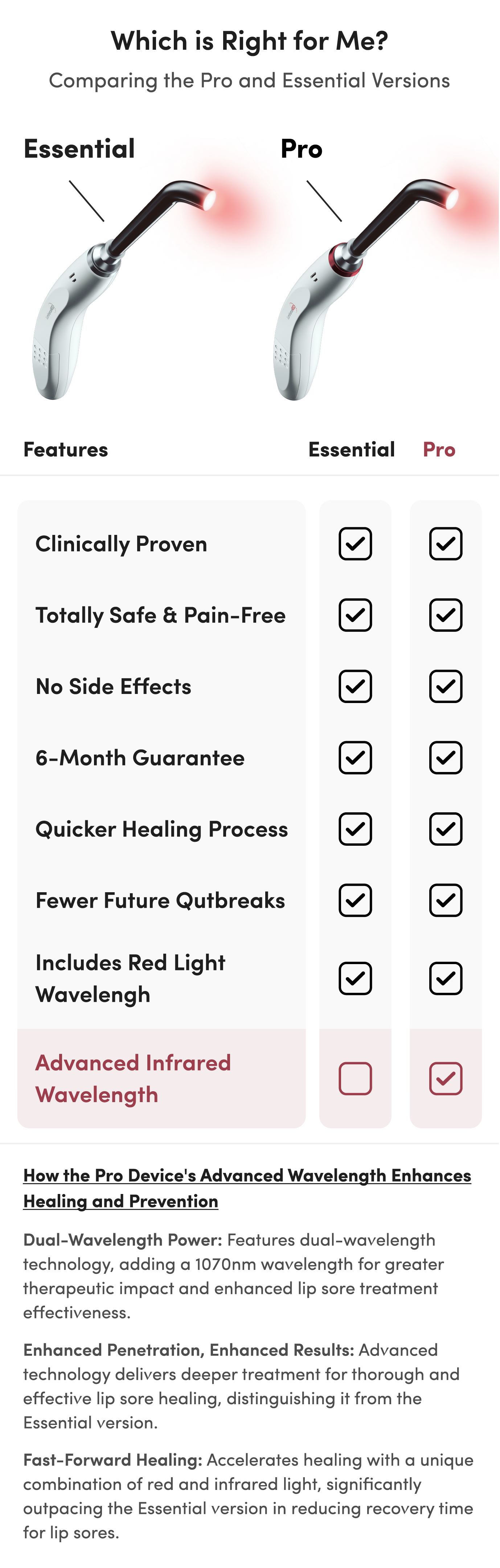
Cold sores don’t usually require medical attention, though you can try a variety of home remedies for them yourself. One natural remedy that has proven very effective for cold sores is treatment with medically-optimized red light. Devices like the Luminance RED offer a simple way for you to try this on your cold sores at home.
But if your cold sore is swelling, causing intense pain or triggering other troubling side effects, it’s probably time to see a doctor.
These symptoms indicate that your cold sore outbreak may be caused by a more serious issue that requires medical attention:
- Severe and painful side effects
- Cold sore that hasn’t healed within 10 days
- Swollen gums
- Weakening immune system
You should also consult a doctor if you’re experiencing COVID-19 symptoms in addition to your cold sores. If you have trouble breathing, persistent pressure in the chest, confusion, low blood oxygen or bluish lips, you should seek emergency medical attention right away.